MCL Injury
MCL Injury
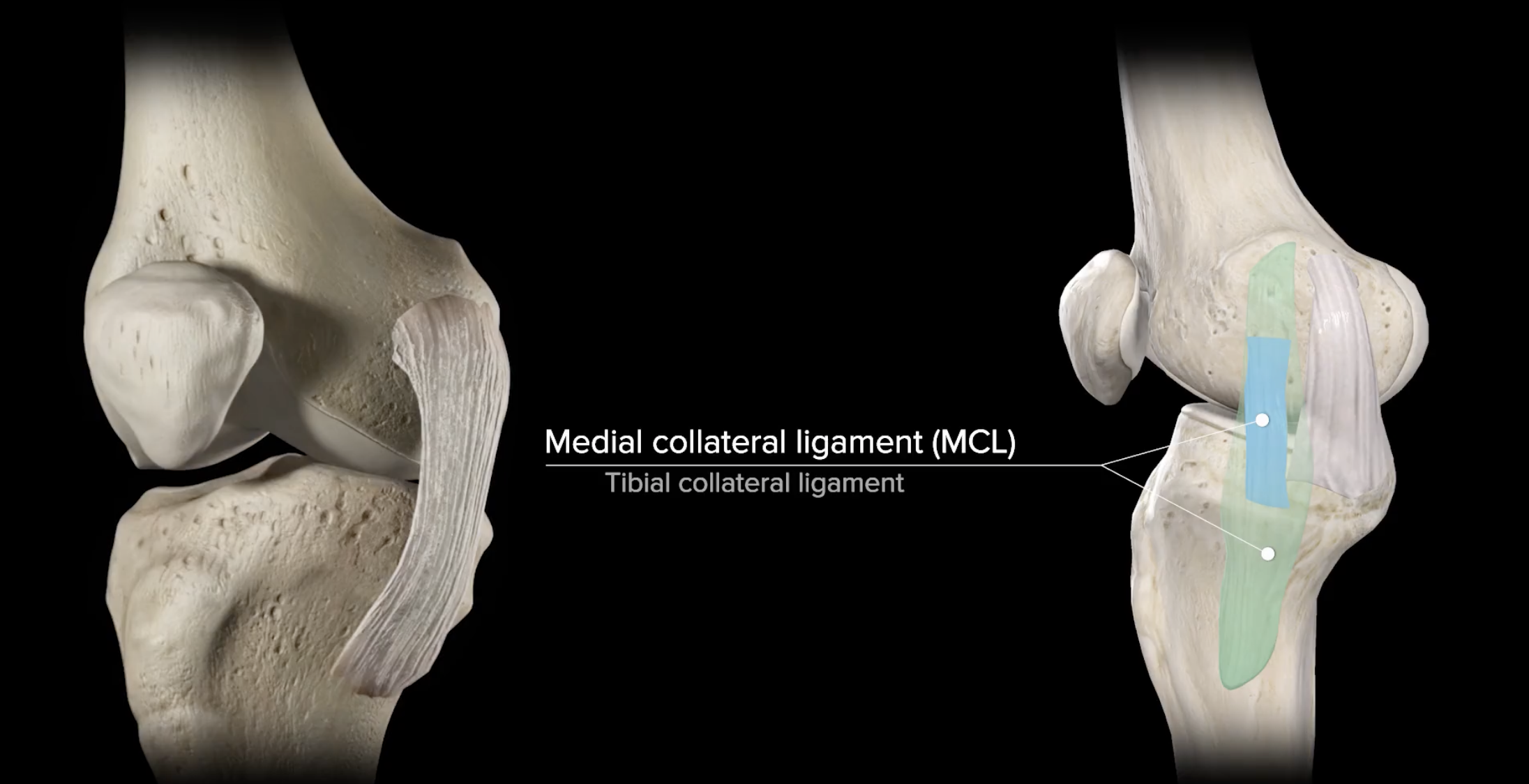
There are four major ligaments stabilizing the knee. The medial collateral ligament (MCL) travels along the inside (medial aspect) of the knee joint from the medial epicondyle, a bony prominence on the inner femur (thigh bone), to the medial condyle, a bony prominence on the inner tibia (shin bone). The MCL, in concert with the lateral collateral ligament (LCL), functions to provide stability to the knee with lateral side-to-side movements. The MCL is not as widely known as the anterior cruciate ligament (ACL), yet it is the most injured of the ligaments within the knee. An injury to the MCL is caused by a substantial force placed along the outer knee causing the knee joint to shift medially resulting in the MCL stretching or becoming partially or completely torn. MCL injuries are most common among athletes that participate in contact sports, such as football, soccer, or wrestling.
Orthopedic Surgeon and Sports Medicine specialist, Dr. Jonathan Koscso, successfully diagnoses and treats patients in Sarasota, FL and the surrounding Gulf Coast region who have experienced a knee MCL injury.
Types of MCL Injuries
Ligament injuries are typically graded on the amount of damage imposed on the ligament. MCL injuries are no different and are assigned to one of three classifications after evaluation of the injury.
Grade 1: The ligament is simply pulled or stretched, so minimal damage is inflicted and the joint remains stable.
Grade 2: The injury results in a partially torn ligament causing mild instability to the knee joint.
Grade 3: The ligament is ruptured and completely torn into two separate pieces. The knee joint is no longer stable with a complete MCL tear.
Symptoms of MCL Injury
The symptoms of an MCL tear are consistent with a number of other knee conditions, so it is important to consult an orthopedic knee specialist for a proper diagnosis. Common complaints of an MCL injury are as follows:
Pain along the inside of the knee immediately following an injury
Tenderness and swelling along the inner portion of the knee
Decreased range of motion
Knee instability, especially with more severe tears
“Locking” or “catching” of the knees with movement
To diagnose a MCL injury, Dr. Koscso will perform a comprehensive medical history and physical examination of the knee. Radiographs of the knee will be taken to ensure no bony injuries such as fractures. The best tool for confirming the diagnosis is magnetic resonance imaging (MRI). This diagnostic tool allows Dr. Koscso to visualize the soft tissue structures within the knee complex and identify if any of these structures also sustained damage with the traumatic event.
Non-Surgical Treatment of MCL Injuries
Patients that have been diagnosed with grade 1 or grade 2 MCL injuries can be treated with conservative therapies alone. The application of a knee brace can help protect the injured ligament during the healing process. Non-steroidal anti-inflammatory medications in combination with RICE (rest, ice, compression, elevation) can be used for pain management and decrease the swelling associated with this condition. A physical rehabilitation program to restore function and stability to the knee joint may also be recommended once the pain and swelling dissipate.
Surgical Treatment of MCL Injuries
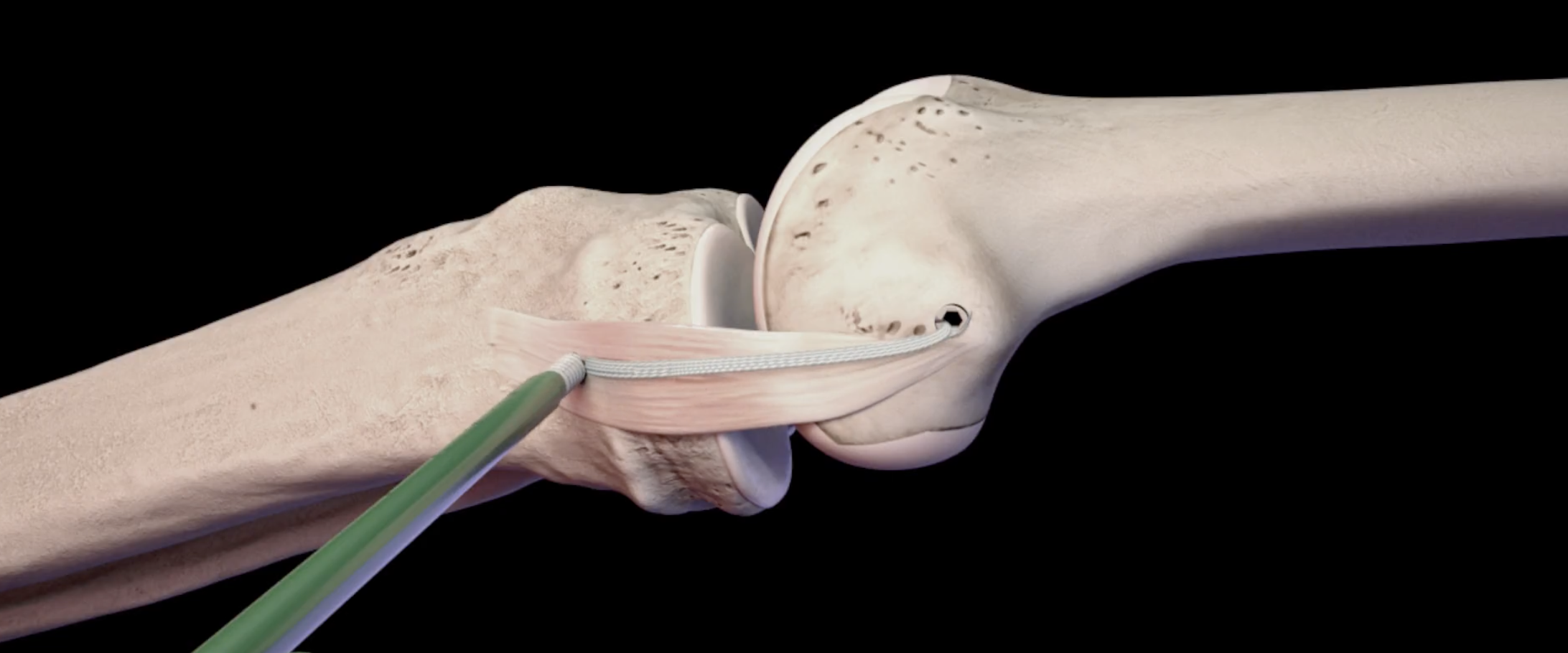
When conservative therapy is unsuccessful, or if a patient experiences a more severe MCL tear, Dr. Koscso may recommend an MCL repair/reconstruction to restabilize the knee. Specialized surgical instruments, sutures and anchors are then used to suture the ligament back together or securely fasten the ligament to the bone. In the event of significant ligament damage that cannot be repaired, a tissue graft, either from the patient (autograft) or donor (allograft), will be used to reconstruct the MCL through a similar mechanism.
Graphic representation of MCL reconstruction via a tissue graft augmented with a collagen-coated high strength suture tape to reinforce the reconstruction for added protection of the knee.
Post-Operative Recovery
For a comprehensive reading of the expected post-operative recovery, including restrictions, physical therapy progressions, and return to work/sport guidelines after MCL repair/reconstruction surgery, please see our corresponding protocol on our physical therapy protocols page.
About the Author
Dr. Jonathan Koscso is an orthopedic surgeon and sports medicine specialist at Kennedy-White Orthopaedic Center in Sarasota, FL. Dr. Koscso treats a vast spectrum of sports conditions, including shoulder, elbow, knee, and ankle disorders. Dr. Koscso was educated at the University of South Florida and the USF Morsani College of Medicine, followed by orthopedic surgery residency at Washington University in St. Louis/Barnes-Jewish Hospital and sports medicine & shoulder surgery fellowship at the Hospital for Special Surgery in New York City, the consistent #1 orthopaedic hospital as ranked by U.S. News & World Report. He has been a team physician for the New York Mets, Iona College Athletics, and NYC’s PSAL.
Disclaimer: All materials presented on this website are the opinions of Dr. Jonathan Koscso and any guest writers, and should not be construed as medical advice. Each patient’s specific condition is different, and a comprehensive medical assessment requires a full medical history, physical exam, and review of diagnostic imaging. If you would like to seek the opinion of Dr. Jonathan Koscso for your specific case, we recommend contacting our office to make an appointment.