Shoulder Osteoarthritis
Shoulder Osteoarthritis
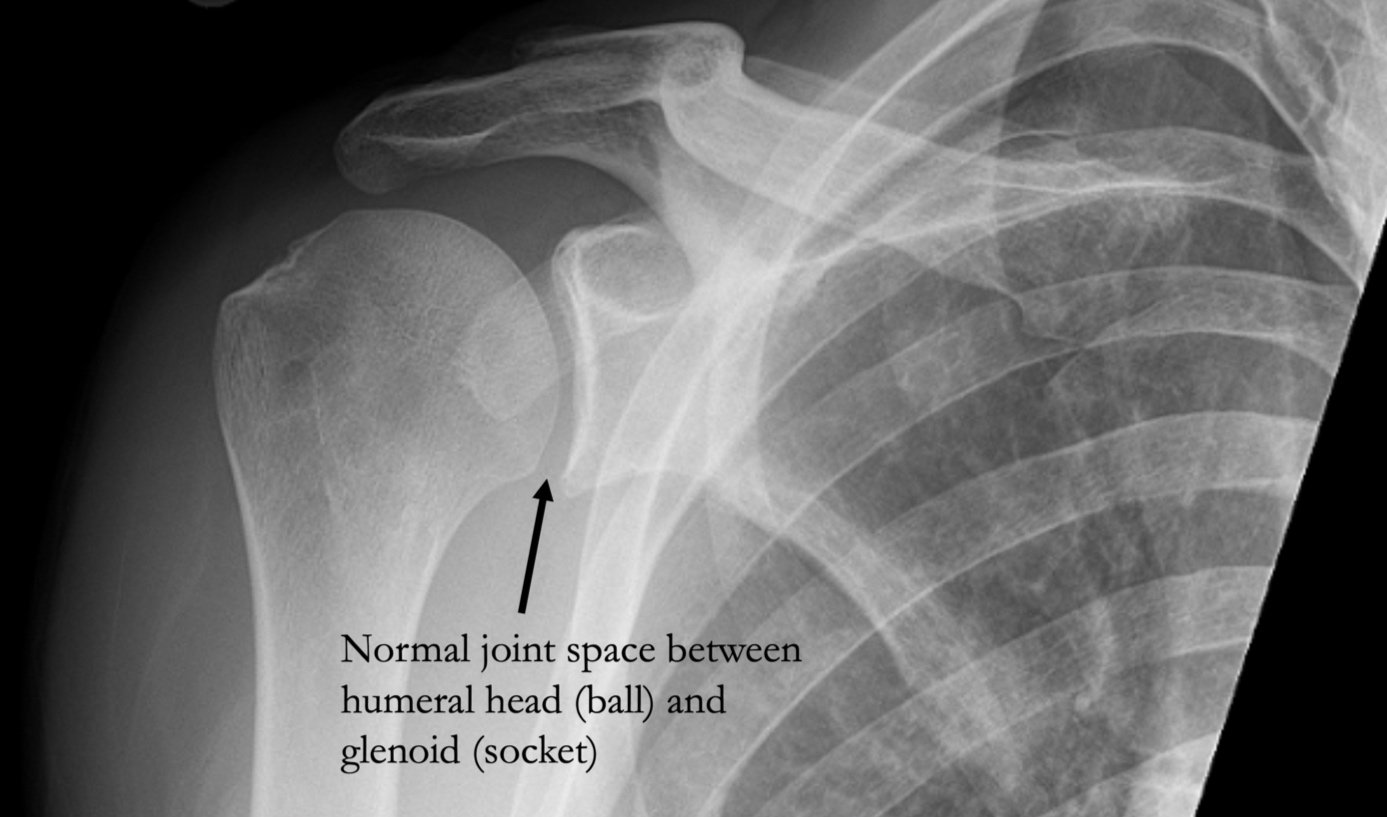
As with other joints in our body, optimal function of the shoulder joint requires a smooth frictionless articulating interface. This surface is provided by normal cartilage at the ends of our bones. Meanwhile, arthritis is a broad term that essentially means inflammation of a joint due to loss of cartilage and all of the subsequent associated changes. Since cartilage does not show up on X-ray, a shoulder joint with normal cartilage and no arthritis will appear to have a gap between the humeral head (ball) and glenoid (socket) on X-ray.
Causes of Osteoarthritis
While the exact cause of arthritis is unknown and is different from person to person, in most instances, the common initial trigger is cartilage injury or loss. In cases of what is termed “secondary” arthritis, this cartilage damage can be related to a previous shoulder dislocation, injury, infection, and surgery, among other causes.
More commonly, patients present with what is termed “primary” arthritis, which is development of arthritis in the absence of the causes listed above. There are multiple theories about why some people develop primary shoulder arthritis. From a genetic standpoint, people with a strong family history of arthritis or a history of arthritis themselves in other joints in the body may be more likely to develop shoulder arthritis. In addition, development of arthritis may be associated with a history of repetitive use and loading of the shoulder joint over a long period of time, such as heavy manual labor or high level weight lifting.
Adaptations to Osteoarthritis
As the process of arthritis progresses, continued loss of cartilage will lead to narrowing and eventual complete loss of joint space as seen on X-ray. This is sometimes referred to as “bone-on-bone” arthritis. With continued cartilage degradation, there is no longer a smooth frictionless surface with shoulder motion and activity. As you can imagine, as joint surfaces become fissured and roughened due to arthritis, like grinding two pieces of sandpaper against one another, continuing shoulder activity and motion leads to inflammation of the joint.
This inflammation is the cause of pain associated with shoulder arthritis. The body has a remarkable way of adapting to disease processes, and in the case of shoulder arthritis, the body attempts to limit shoulder motion in several ways. First, the soft tissue capsule around the shoulder becomes thickened and contracted to stiffen the shoulder joint. Second, bone spurs, also referred to as osteophytes, form around the joint to further reduce motion.
Orthopedic Surgeon and Sports Medicine specialist, Dr. Jonathan Koscso, successfully diagnoses and treats patients in Sarasota, FL and the surrounding Gulf Coast region who are experiencing shoulder osteoarthritis.
Symptoms of Shoulder Osteoarthritis
Patients with shoulder arthritis most commonly experience pain and stiffness in the shoulder. The location of pain can vary from patient to patient, but most people report feeling a deep-seated pain within the joint. Initially the pain occurs primarily with high-demand activities and certain shoulder positions, but as the disease progresses, pain can occur with more and more activities of daily living. With moderate to severe shoulder arthritis, pain then frequently occurs at night that can interfere with sleep. In fact, night-time pain and poor sleep is the most common reason why patients seek consultations with our office.
Non-Surgical Treatment of Shoulder Osteoarthritis
As with other chronic shoulder conditions, we recommend beginning with non-operative treatment. The primary objective is to reduce inflammation, which can be accomplished through activity modification, oral anti-inflammatory medications (NSAIDs, i.e. ibuprofen, naproxen, meloxicam, etc.), oral corticosteroids, corticosteroid (cortisone) injections, and biologic injections such as platelet-rich plasma (PRP). Physical therapy can be helpful in correcting any negative functional or postural adaptations you have made due to shoulder pain. We offer all of these treatments at Kennedy-White Orthopaedic Center, and every patient’s response to the various options is different. While none of these treatments actually reverse the progression of arthritis, however, they can provide pain and symptom relief for long periods of time.
Surgical Treatment of Shoulder Osteoarthritis
If non-operative treatment methods have failed to provide lasting symptom relief, then surgical treatment may be offered. Depending on the patient’s individual constellation of symptoms and imaging findings, there may be a role for a joint-preserving, minimally-invasive arthroscopic procedure called Comprehensive Arthroscopic Management (CAM). This procedure consists of thorough arthroscopic debridement of the shoulder, removal of any loose bodies in the joint, capsular release and removal of humeral head osteophytes (bone spurs) to improve shoulder range of motion, subacromial decompression to remove any bone spurs above the rotator cuff, and biceps tenodesis to eliminate the biceps tendon as a pain generator. This may be a potential option for the young, active patient with mild to moderate shoulder arthritis that wants to preserve their shoulder for as long as possible, with the understanding that this procedure in no way restores cartilage or reverses the process of arthritis. We would be happy to discuss this option with you during your consultation.
Ultimately, the definitive treatment for end-stage shoulder arthritis is total shoulder arthroplasty (replacement). This involves replacing the arthritic humeral head (ball) with a metal implant, and the glenoid (socket) with a highly cross-linked polyethylene plastic liner.
This type of shoulder replacement is called anatomic total shoulder replacement, because the native humeral head (ball) is replaced by an implant with a spherical surface, and the native glenoid (socket) is replaced with an artificial socket. Optimal outcomes after anatomic total shoulder replacement requires a well-functioning rotator cuff, which will be confirmed by Dr. Koscso pre-operatively based on physical examination and/or imaging.
Overall, anatomic total shoulder replacement provides consistently excellent outcomes in terms of pain relief, functional improvement, and longevity. In the right patient, Dr. Koscso typically uses an innovative bone-preserving technique with a “stemless” implant, which uses cutting-edge porous-coating material science to eliminate the need to remove more of your native healthy bone. We will discuss whether this could be an option for you at your appointment.
Recovery After Shoulder Replacement Surgery
For a comprehensive reading of the expected post-operative recovery, including restrictions, physical therapy progressions, and return to work/sport guidelines after anatomic shoulder replacement surgery, please see our corresponding protocol on our physical therapy protocols page.
About the Author
Dr. Jonathan Koscso is an orthopedic surgeon and sports medicine specialist at Kennedy-White Orthopaedic Center in Sarasota, FL. Dr. Koscso treats a vast spectrum of sports conditions, including shoulder, elbow, knee, and ankle disorders. Dr. Koscso was educated at the University of South Florida and the USF Morsani College of Medicine, followed by orthopedic surgery residency at Washington University in St. Louis/Barnes-Jewish Hospital and sports medicine & shoulder surgery fellowship at the Hospital for Special Surgery in New York City, the consistent #1 orthopaedic hospital as ranked by U.S. News & World Report. He has been a team physician for the New York Mets, Iona College Athletics, and NYC’s PSAL.
Disclaimer: All materials presented on this website are the opinions of Dr. Jonathan Koscso and any guest writers, and should not be construed as medical advice. Each patient’s specific condition is different, and a comprehensive medical assessment requires a full medical history, physical exam, and review of diagnostic imaging. If you would like to seek the opinion of Dr. Jonathan Koscso for your specific case, we recommend contacting our office to make an appointment.