Shoulder Instability
Shoulder Instability / Labrum Tear
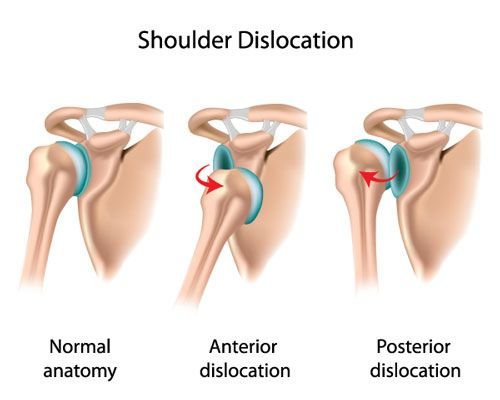
The shoulder joint has very little inherent bony stability, and relies heavily on static and dynamic soft tissue stabilizers such as the labrum, capsule, and surrounding muscles and tendons. Relative to other joints in the body, the shoulder socket (glenoid) is relatively shallow- somewhat like a golf tee. The humeral head rests upon the glenoid somewhat like a golf ball on the tee. With enough trauma to the shoulder, such as through contact sports, skiing or snowboarding, motor vehicle accidents, or even just a slip and fall from standing, the humeral head can sublux (slide out of position) or dislocate from the glenoid. Subluxation, which is when the shoulder partially but not fully comes out of position, typically reduces (go back into position) on its own. In contrast, full shoulder dislocations, particularly first-time dislocations, may require a trip to the emergency room to be reduced.
Orthopedic Surgeon and Sports Medicine specialist, Dr. Jonathan Koscso, successfully diagnoses and treats patients in Sarasota, FL and the surrounding Gulf Coast region who have experienced shoulder instability.
For a detailed illustration of the relevant anatomy involved in a shoulder dislocation, the below video is quite helpful.
Shoulder Instability in the Young Athlete
Almost by definition, the shoulder labrum and joint capsule must be torn for a shoulder to dislocate. The labrum is a critical cartilaginous structure that circumferentially lines the glenoid (socket) to help prevent the humeral head (ball) from sliding out of place - similar in nature to the bumpers on a pool table. In the majority of shoulder dislocations, the humeral head comes out in front of the glenoid. Therefore, the anterior shoulder labrum and capsule will be torn, and this tear is referred to as a "Bankart lesion”.
Bankart lesion seen during arthroscopic surgery of a right shoulder. Humeral head (ball) is above, and glenoid (socket) is below. Note the detachment and redness of the labrum as it is separated from the glenoid rim.
In more severe cases or with multiple dislocations, injury to the bony structures can also occur. On the humeral head (ball) side, as it dislocates over the rim of the glenoid (socket), the humeral head can be impacted against the glenoid rim, thus creating a divot in the humeral head surface. This defect is called a “Hill-Sachs lesion”. On the glenoid (socket) side, bony injury to the lip of the glenoid rim can also occur with shoulder dislocation. Sometimes this is referred to as a “bony Bankart lesion”. In more severe cases, this is referred to as “glenoid bone loss”, and any loss of bone in this critical area significantly reduces the stability of the shoulder joint.
In a young athlete with shoulder instability and dislocation, the treatment decision-making hinges entirely around the risk of additional dislocations and instability events. The goal of treatment is to avoid repeated dislocations, as the high amount of shear stresses on the cartilage surface during dislocation may predispose the shoulder to developing early arthritis in the future.
Thankfully, there is a large amount of high-quality published data to inform our decision-making process. We know that there are a number of risk factors associated with re-dislocation, including younger age, participation in contact sports, and overall ligamentous laxity. In fact, in a young athlete with the above risk factors, even after just a single shoulder dislocation, the risk of the shoulder dislocating again can be as high as 90% without surgery. Conversely, in an older patient that does not participate in contact sports, the risk of re-dislocation can be quite low.
Shoulder Instability in the Older Adult
As discussed above, the risk of re-dislocation in the older adult can be quite low, and recurrent instability is generally not the primary concern. Rather, shoulder dislocations in patients over the age of 40 is associated with acute rotator cuff tears. This would manifest as pain and weakness that persist even after the shoulder joint has been reduced. In this patient population, if there is any concern about the rotator cuff based on your symptoms and physical examination, we would likely recommend an MRI to carefully assess for a rotator cuff injury.
Treatment of Shoulder Instability / Labrum Tear
As you have likely intuited based on the information thus far, treatment of shoulder instability is highly specific and personalized to each individual patient. For a high school football player that wants to continue playing football, perhaps at the collegiate level in the future, we may recommend surgery after a single first-time shoulder dislocation. Meanwhile, for a 33-year-old accountant who dislocated their shoulder while water-skiing for the first time (and who is not particularly interested in water-skiing again after this experience), we would likely recommend non-operative treatment and rehabilitation with physical therapy.
For patients planning to undergo surgical stabilization of the shoulder, the procedure itself can vary tremendously from patient to patient as well. For a first-time shoulder dislocation with an isolated soft tissue injury (Bankart lesion) and no associated bone loss, surgical stabilization would likely entail minimally-invasive arthroscopic repair of the injured capsule and labrum. On the other end of the spectrum, to surgically stabilize a shoulder with significant bone loss in addition to soft tissue injury, surgery would likely involve reconstructing the bony defect through transferring the nearby coracoid bone (Latarjet procedure), transferring bone from elsewhere in the body, or a bone transplant from a cadaveric donor (allograft).
Arthroscopic shoulder stabilization with labral repair
Again, we believe that treatment for shoulder instability must be customized for each individual patient based on your unique injury severity, risk factor(s), age, activity level, occupation, and expectations. As a sports-focused practice, we are equipped to provide whichever treatment is the best for you. At your consultation, Dr. Koscso will carefully review your injury history, symptoms, physical examination, and imaging to arrive at a treatment plan with you.
Recovery After Shoulder Stabilization / Labrum Repair
For a comprehensive reading of the expected post-operative recovery, including restrictions, physical therapy progressions, and return to work/sport guidelines after shoulder stabilization surgery, please see our corresponding protocol on our physical therapy protocols page.
About the Author
Dr. Jonathan Koscso is an orthopedic surgeon and sports medicine specialist at Kennedy-White Orthopaedic Center in Sarasota, FL. Dr. Koscso treats a vast spectrum of sports conditions, including shoulder, elbow, knee, and ankle disorders. Dr. Koscso was educated at the University of South Florida and the USF Morsani College of Medicine, followed by orthopedic surgery residency at Washington University in St. Louis/Barnes-Jewish Hospital and sports medicine & shoulder surgery fellowship at the Hospital for Special Surgery in New York City, the consistent #1 orthopaedic hospital as ranked by U.S. News & World Report. He has been a team physician for the New York Mets, Iona College Athletics, and NYC’s PSAL.
Disclaimer: All materials presented on this website are the opinions of Dr. Jonathan Koscso and any guest writers, and should not be construed as medical advice. Each patient’s specific condition is different, and a comprehensive medical assessment requires a full medical history, physical exam, and review of diagnostic imaging. If you would like to seek the opinion of Dr. Jonathan Koscso for your specific case, we recommend contacting our office to make an appointment.