Rotator Cuff Tear
Rotator Cuff Tear
As discussed in our shoulder anatomy page, the rotator cuff is a set of 4 muscles and tendons around the shoulder that serves two purposes:
1) keep the humeral head (ball) centered in the glenoid (socket) through shoulder range of motion, and
2) initiate and maintain certain shoulder movements.
For an illustrative demonstration of the biomechanics of the rotator cuff muscles and their respective injuries, the below video is quite helpful.
The rotator cuff consists of four muscles - subscapularis in the front (anterior), supraspinatus on top (superior), and infrapinatus and teres minor in the back (posterior). These muscles all arise from the scapula (shoulder blade) and attach on the humeral head.
Acute Rotator Cuff Tear
With a significant trauma to the shoulder, even a previously normal rotator cuff can be acutely torn. Typically patients will report immediate onset of pain in the shoulder, followed by weakness, that is not getting better on its own. In patients over the age of around 40, acute rotator cuff tears are associated with shoulder dislocations.
In the setting of an acute rotator cuff tear, surgical repair in a relatively timely fashion is generally recommended. If left unrepaired for a prolonged period of time, a torn rotator cuff will progressively retract, as the muscle continues to pull on a tendon that is not attached to anything. In addition, the muscle will undergo atrophy and fatty infiltration, a process in which previously healthy muscle is irreversibly replaced by non-functional fatty tissue.
Chronic Rotator Cuff Tear
Much more commonly, we treat patients that have more of a chronic rotator cuff issue. Patients often report a long duration of mild but progressively worsening symptoms, that might have been exacerbated by an otherwise fairly benign activity, such as a golf swing or reaching for something in the backseat of their car. The classic presentation of rotator cuff pain includes pain at the side of the shoulder that can radiate down to the elbow, pain and weakness with overhead activities and lifting away from the body, and most importantly, night pain that interferes with sleep. In fact, night pain is probably the No. 1 reason that patients decide to come see a shoulder doctor.
Why is rotator cuff disease so common as patients get older? There is a multitude of reasons, but it is helpful to categorize them into intrinsic and extrinsic factors that lead to degeneration of the tendon(s) and eventual tear.
Intrinsic degeneration
Like other collagen-containing structures in our body, tendon degeneration is part of the aging process. Just like our skin, our rotator cuff tendons lose water content and elasticity as we age. This reduces the tendon’s ability to fully recover and heal from the constant micro-trauma that occurs from recreational and daily activities. The repetitive damage then accumulates until the tendon becomes structurally altered and weakened, thus making it vulnerable to tearing even with very minor loads.
Extrinsic damage
The other etiologic category for chronic rotator cuff degeneration includes tendon damage due to factors external to the biology within the tendon. In particular, the supraspinatus, which is the rotator cuff tendon at the top of the shoulder, lives in a relative tight space between the humeral head and the undersurface of the acromion bone. This space is called the subacromial space. Every time you lift your arm up above your shoulder, the subacromial space becomes smaller and the supraspinatus tendon gets compressed or pinched against the undersurface of the acromion. Over time, this repetitive pinching can damage the tendon.
Further worsening this problem, over years of repetitive use with sports, work, recreation, and activities of daily living, the body adapts to this impingement by forming extra bone - otherwise known as a bone spur - under the acromion, which exacerbates the problem and thus initiating a vicious cycle.
This process of chronic rotator cuff disease occurs along a spectrum, beginning with subacromial impingement and bursitis (inflammation), rotator cuff tendinitis, to partial rotator cuff tears, and finally to full-thickness rotator cuff tears.
Treatment of Rotator Cuff Tears
Nonoperative Treatment
First, not all rotator cuff tears need to be treated. In fact, if you did MRI scans on patients over the age of 50 with no shoulder symptoms, a significant percentage of patients would have rotator cuff tears and not even know about it. However, if you are coming to our office with shoulder pain, and your symptoms, physical exam, and imaging are all consistent with rotator cuff disease, then we would likely offer treatment to reduce your pain and improve function.
Unless you have an acute traumatic rotator cuff tear, for most patients with more chronic rotator cuff pathology, we generally begin with non-operative treatment. The majority of patients actually respond very well to non-operative treatment and avoid surgery entirely. These treatments are aimed at reducing inflammation, which is the source of pain, and improving the function of the shoulder through physical therapy.
Reduction of inflammation can be achieved through a combination of activity modification, oral anti-inflammatory medications (NSAIDs, such as ibuprofen, naproxen, meloxicam, etc.), and injections. For most patients, a corticosteroid (i.e. cortisone) injection can be highly effective at reducing pain and inflammation, and can last for a period of weeks to months. Platelet-rich plasma (PRP) is another option for reducing inflammation, with the advantage of avoiding the potentially deleterious effect on tendon health associated with multiple cortisone injections.
Strengthening the muscles around the shoulder through a physical therapy regimen is also critical to a successful nonoperative treatment plan. Patients with rotator cuff disease often have several muscle imbalances that position the shoulder blade in a way that contributes to or worsens the pathology. Proper physical therapy is aimed at correcting these muscle imbalances as well as strengthening the other muscles around the shoulder that provide mobility for daily use and sporting activity.
Operative Treatment
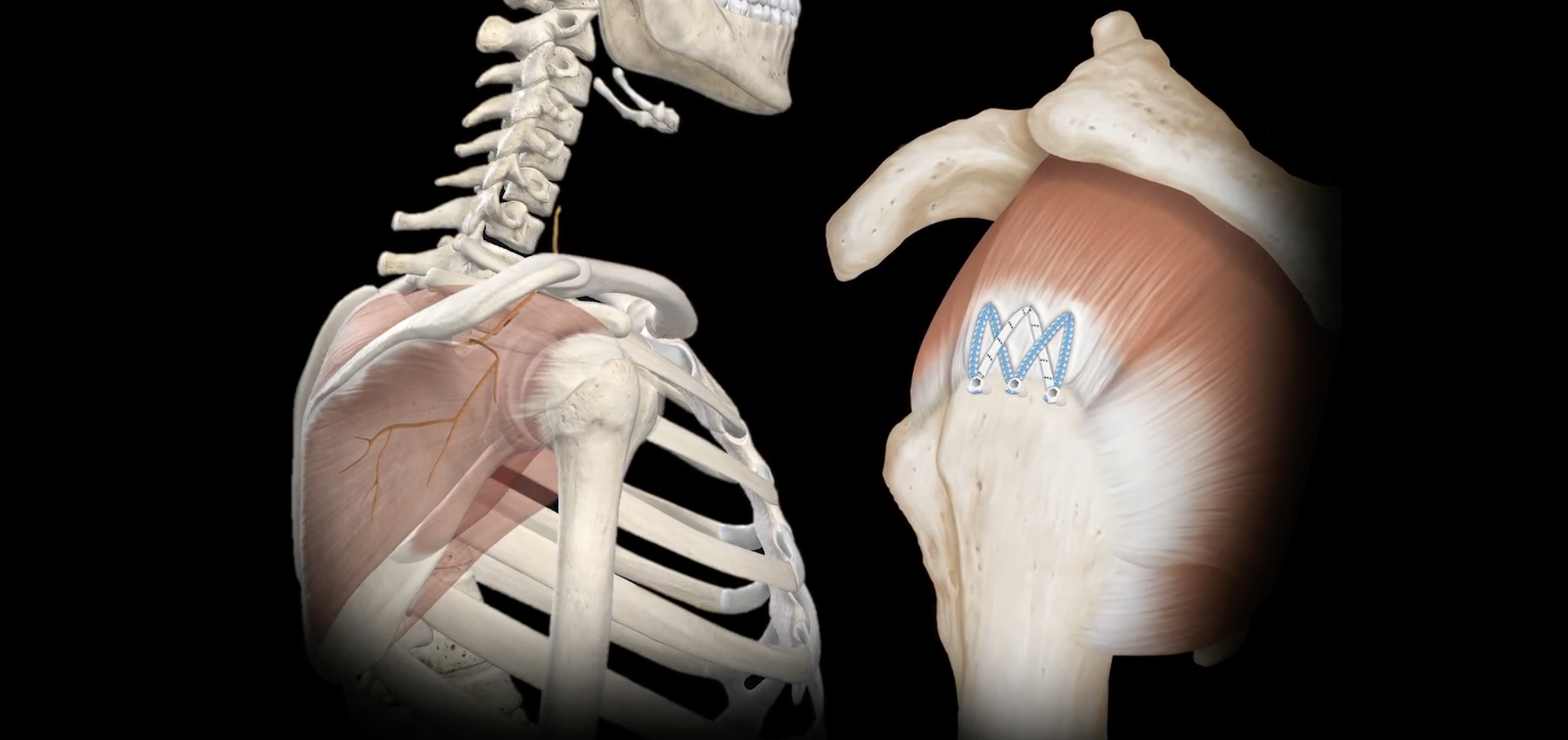
If your shoulder symptoms continue to persist despite trials of non-operative treatment, then we may recommend rotator cuff repair surgery. This is typically performed with a minimally-invasive arthroscopic approach. Any other issues in the shoulder, such as subacromial bone spurs, acromioclavicular (AC) joint arthritis, or biceps tendon disease would all be addressed during surgery. We will review the risks, benefits, post-operative recovery, rehabilitation, and any other questions you may have in detail during a pre-operative discussion with Dr. Koscso.
Arthroscopic rotator cuff repair - before (left), after repair (right).
Post-Operative Recovery
For a comprehensive reading of the expected post-operative recovery, including restrictions, physical therapy progressions, and return to work/sport guidelines after rotator cuff repair surgery, please see our corresponding protocol on our physical therapy protocols page.
About the Author
Dr. Jonathan Koscso is an orthopedic surgeon and sports medicine specialist at Kennedy-White Orthopaedic Center in Sarasota, FL. Dr. Koscso treats a vast spectrum of sports conditions, including shoulder, elbow, knee, and ankle disorders. Dr. Koscso was educated at the University of South Florida and the USF Morsani College of Medicine, followed by orthopedic surgery residency at Washington University in St. Louis/Barnes-Jewish Hospital and sports medicine & shoulder surgery fellowship at the Hospital for Special Surgery in New York City, the consistent #1 orthopaedic hospital as ranked by U.S. News & World Report. He has been a team physician for the New York Mets, Iona College Athletics, and NYC’s PSAL.
Disclaimer: All materials presented on this website are the opinions of Dr. Jonathan Koscso and any guest writers, and should not be construed as medical advice. Each patient’s specific condition is different, and a comprehensive medical assessment requires a full medical history, physical exam, and review of diagnostic imaging. If you would like to seek the opinion of Dr. Jonathan Koscso for your specific case, we recommend contacting our office to make an appointment.